The DRA Dilemma - Myths & Truths.
We are wrapping up the month of July which is Diastasis Recti Abdominus (DRA) awareness month. This post will be all about DRA - what is it, what's normal, and what the hell the DRA dilemma is -- and why YOU should care. There is so much misinformation out there which is farther contributing to this dilemma. My intent is to be a trusted resource for all -- what I am writing in this post is:
research-based
current best treatment approaches
what is being utilized by the top pelvic health physical therapists in the WORLD.
And before we get started, I want to be upfront and honest with you. There is a lot we still do not know about DRA. The good news is, there are so amazingly smart and incredibly talented individuals who are leading the way on a better understanding of this condition.
First up, what is DRA?
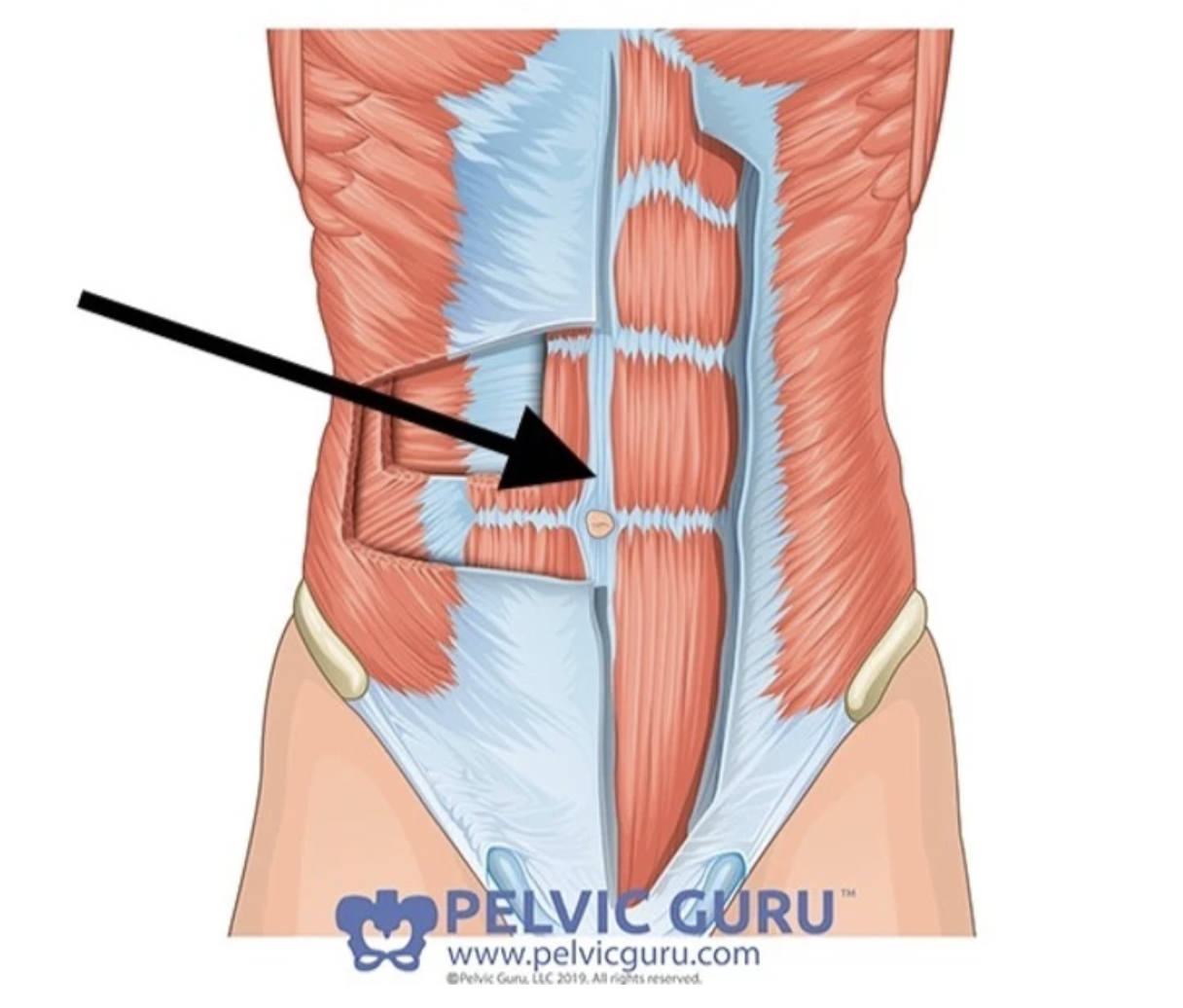
Diastasis recti in it's purist definition is a thinning, weakness, and/or lack of stiffness of the linea alba which is the connective tissue between the "6-pack" muscles of the core - the rectus abdominus (see black arrow in picture below which demonstrates the linea alba).
How do I know if I have one?
The gold standard diagnosis for a DRA is performed with an ultrasound image. Some physical therapists have a diagnostic ultrasound in their clinic, however they are mostly utilized with research.
Traditionally, DRA is assessed with the supine (laying on your back), head lift test. This is where you would lay on your back and lift your head/shoulders slightly off the floor/table. In this position, we would palpate along that the linea alba from the sternum to the pubic bone. We are assessing:
Width of the two rectus bellies (rectus abdominus muscles from left and right sides). This is measured by either fingertip width, or with a measuring tape. This is also termed inter-recti distance (or IRD). When you lift your head the left rectus belly and the right rectus belly become active and close in towards each other. When there is two fingertip width or more between the left and right rectus bellies, (2.5cm or about 1 inch), then it is considered a DRA.
Depth, or how deep is the "separation" usually measured by landmarks on one's finger (ie. to nail, to DIP joint, PIP joint, etc). Most PTs knowing the length of these landmarks on their finger, so the depth can be also recorded in centimeters.
Stiffness or tension is measured based on how much "give" the linea alba provides. Is it soft/squishy (less tension) or does it feel like a trampoline (more tension).
Presence of abdominal bulge/distention/coning. (FYI:there are different words for this and based on which expert to talk to, these can all mean the same thing, or different things. For the purpose of this blog post, I am going to combine them into one). Essentially, we are looking at the function of that DRA - are you able to manage pressure well when you stress the tissue (with the head lift) -- ie. tension, core activation. Or do you have challenges with this and thus have an abdominal bulge/mommy tummy etc.
You should be assessed with palpation and observation in multiple positions and movements since we do not "live" in the supine position! If you are seeing a healthcare provider that is only assessing the width, and only in the supine position -- run! Run away! That is the outdated way of assessing DRA.
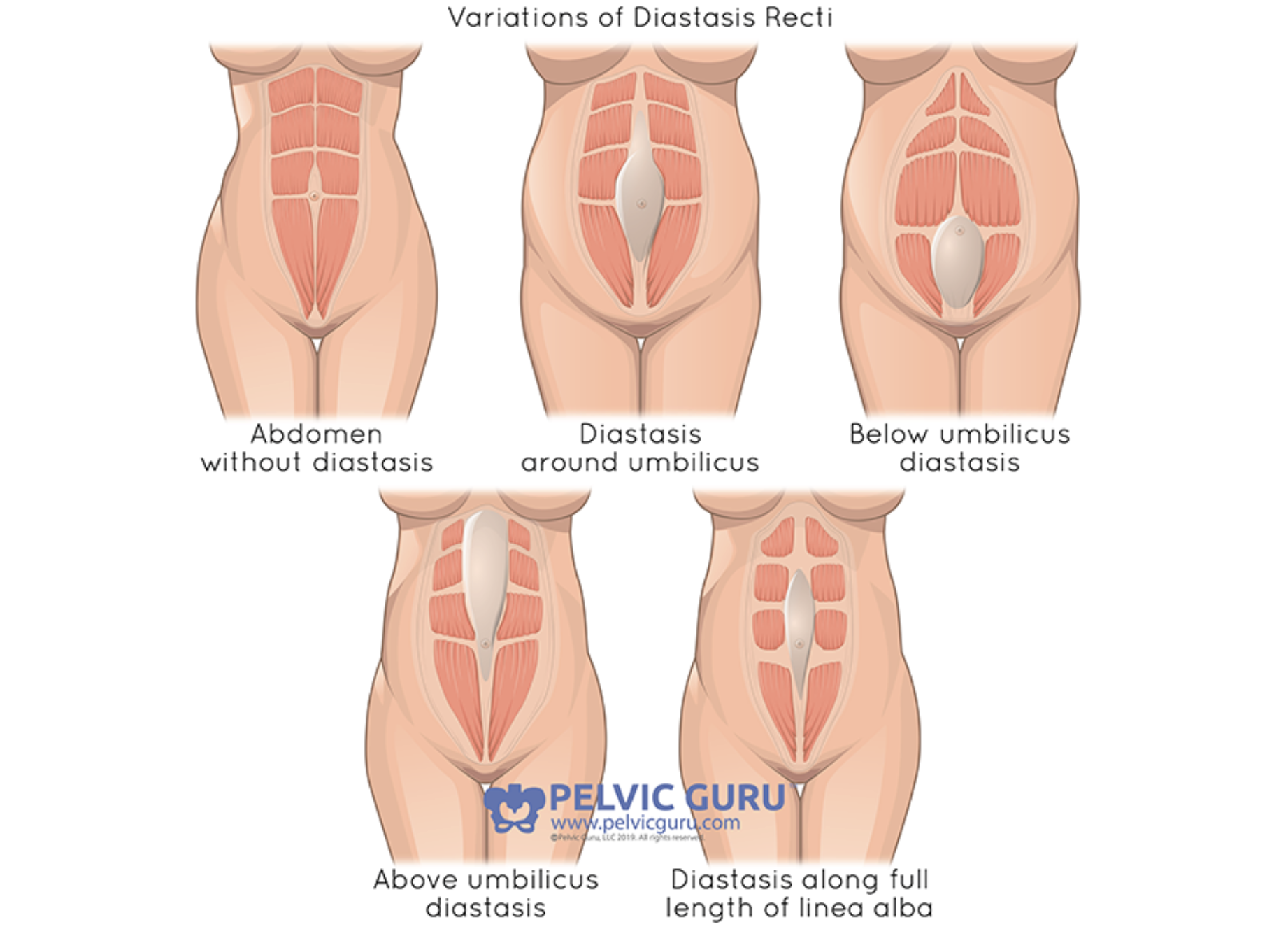
Here are some examples of a DRA:
(Permission to use copyright image from Pelvic Guru, LLC pelvicguru.com)
How common is this?
DRA is very common- studies have found between 66-100% of women by full-term pregnancy (ie. the day that they give birth) have one! So what I'm saying is that it is NORMAL for the abdominal muscles including the connective tissue and fascia to elongate and become less stiff. Our entire abdomen from front to back and side to side is growing, these tissues are made to stretch to allow for this. Our bodies are amazing!
One study found 35-39% postpartum women continued to have a DRA at 6 months postpartum. for the 3-4/10 women who continue to have a DRA at 6 months, that does not necessarily mean that did/are doing "harm". Connective tissue TAKES TIME to heal and strengthen, much longer than muscle which typically takes 6-8 weeks. Studies have actually found that the muscle and connective tissue in postpartum women takes on average 9-12 months. (I'm so sorry mommas that our healthcare system is sending you back into the movement/exercise world at six-weeks with no knowledge of this!)
DRA is not just limited to women during pregnancy and postpartum. It is very common in children, and can be seen in the aging adult as well. In children, their bodies are much more 'elastic' and mobile since they are growing and changing a ton, thus DRA can be very normal! Older adults who form a DRA, it is often due to poor pressure management systems over the years. I see it often in men, especially those who have that "pot belly" look with a very firm abdomen.
Why doesn't my OB check for this?
This is a great question. One reason why is because they are not the musculoskeletal experts. They do not understand the ends and outs of muscles, connective tissue, ligaments, etc. Their main job is to assess organs/systems of the body such as the reproductive system. Please check out my blog post on the difference between and OB gynecological exam and a pelvic floor assessment here. This is why this information for you to look for a pelvic health physical therapist in your area, for at least one full pelvic health assessment postpartum.
In my area specifically, OBs do not check for a DRA at the 6-week postpartum check-in. Often times you may get a "let's just wait an see" answer. It is never too early or late to start physical therapy, but in an ideal world, those first few months postpartum are an excellent time to start.
Is DRA the same thing as mommy tummy?
I get this question a lot -- "I am exercising and I still have that 'mommy tummy' or 'belly bulge' look. Is this a DRA?" Based on the true definition of a DRA-- the separation/laxity of the linea alba thus increased intra-recti distance > 2.5cm (or two fingertips width), the answer is maybe?
What I tend to see MORE than a true DRA is:
weakness of the lower core
over-utilizing the upper core muscles
poor breathing mechanics
poor postural awareness
decreased hip/gluteal strength/coordination and endurance
poor pressure management strategies
These can all lead to a 'mommy tummy'. And guess what? All of these things can be 'fixed'. They just take time!
Could my DRA be the cause of my __________ ?
Fill in that blank with low back pain, neck/upper back pain, SI pain, pelvic pain, incontinence, etc. So the evidence is definitely mixed on this one. Most recent studies have found that there is not a connection between DRA and low back pain and/or pelvic girdle pain, or incontinence. This can be apart of that DRA dilemma as there are many different ways that a DRA is being diagnosed and thus treated. In truth, low back pain is very common! 80% of people will suffer from low back pain at some point. So can the low back pain be connected? Maybe? But one "weak point" in the linea alba in the front of the abdomen is just ONE part of the entire body system. To specifically focus on only this is part of the problem. Do you have a 2 finger DRA but no bulging, no pain/dysfunction, good awareness, good coordination, not limited with your daily activities? Then your DRA is probably normal! (FYI: I have a DRA based on the true definition, and I've never had children. This is my normal.)
Do you have GI distress, or pubic bone pain, or upper back pain, or difficulty with connecting with your core AND you have bulging? Okay perhaps there is a dysfunction within the entire core system as a hole and maybe the DRA isn't helping matters. You would be an excellent candidate for an evaluation with a pelvic health physical therapist.
What exercises should I avoid?
This is the next most frequent question that I get. The quickest answer is: there is no such thing as list of "good" and "bad" exercises for DRA. Again, if you have a healthcare provider to personal trainer telling you that you must avoid things like sit ups, rotations, and even planks... RUN, RUN away! This is outdated information that we now know is incorrect. There may be more optimal and less optimal exercises for you specifically. To give you more than just an "it depends" answer, here is my advice:
start with the foundations: breathing, posture awareness, gentle lower core activation, and self care such as management of constipation. I have a seven-part video series of the foundational exercises postpartum that you can start right away. Send me an email at jenniferparker@embodywellnesspt.com to request these FREE videos.
Pay attention to your daily movements, like rolling over in bend, coming from sitting up to standing, washing your hair in the shower, leaning over to change diapers... do you notice a pressure at your abdomen? Any feeling of bulging? If so, see back to point #1- try to engage your lower core before starting these movements, or modify them. I want to re-iterate, and this is very important to know: you are NOT harming yourself when you see an abdominal bulge when you move. I do not want you to feel disempowered to move in your body. The goal is to start to become aware and adjust your daily movements as needed.
If you are performing an exercise and you notice a bulge, before stopping or modifying the exercise- can you see if you can decrease that bulge with improved breath control? With improved coordination of breathing with TrA activation? What about if you check in with your head/neck position? I will admit, this is tough to do on your own. This is where physical therapists can come in or other corrective exercise specialist with advanced knowledge in DRA can help guide you.
This leads to the "DRA Dilemma" which is a term I took from a pelvic health physio (PT) named Munira Hudani. Studies have found that the most benefit strength training program for DRA includes:
progressive exercises
individualized to the person
understanding of how to modify
include functional movements
tensioning the connective tissue of the linea alba
performed most days of the week
can start at day TWO postpartum
Let me pick our a few key words from above:
Individualized: meaning, there is no cookie cutter approach to this. There may be some guidelines out there, but everyone will be different. Simply following an online program may not be enough for some.
Tensioning: Connective tissue needs to be "loaded" or challenged in order for it to heal. So to avoid all exercises that provide a challenge to this core system, more likely to continue said 'mom tum'.
TWO Days postpartum. Say what?? Yep. A study found gentle exercises starting at day two postpartum was far superior to improving core strength than wearing an abdominal binder the first 6 weeks postpartum. Another study compared two different types of progressive exercise program that started at two days postpartum : the first was mostly supine and sidelying deep core strengthening exercises. The other program included both the supine/sidelying core exercises as well as functional movements including squats, lunges and rotation movements. The second group had far superior strength than the first group that remained even a year after the study was finished.
Progressive: meaning it slowly builds. There are lots of ways to modify, advance and challenge this entire core system... slowly. If you put in the work on the foundations first, I promise you won't be less likely to be sidelined with an injury the first few years postpartum and beyond.
I always tell my patients that "you know your body best". If you feel lost and uncertain on where to go, please know that there are providers out there who can help guide and navigate through the confusion of "good/bad". The last thing I would ever want is a momma to be afraid to move. One of my patients told me her OB told her at 6-weeks postpartum with a c-section birth "yes, go back to exercise but be careful not to injury your pelvic floor". This messaging puts out so much fear and anxiety with returning to movement, thus the dilemma. My intention as a pelvic health physical therapist to bridge this gap of confusion, and to work with mommas to get back to the activities that they enjoy without pain or fear.
How do I find a pelvic health PT near me?
There are several credible websites that can be used to find a pelvic health PT near you.
The American Physical Therapy Association (APTA)- Women’s Health Section website has a directory. Link is found here: https://www.womenshealthapta.org
Herman & Wallace Institute provides continuing education for pelvic health. This is the program that I have done the majority of my continuing education courses. They have a wide PT directory which can be found at: https://pelvicrehab.com
The Global Pelvic Health Alliance through @pelvicguru1 has a directory of pelvic health practitioners- including physical therapists, personal trainers, and gynecologists to name a few. Find this directory at https://pelvicguru.com
You can also ask your OB if they have a trust pelvic health PT that they would recommend. Please know, your OB is unlikely to offer information on pelvic health PT unless YOU ask. Or ask your local mom groups, doula groups, close friends, etc.